High Blood Pressure (Hypertension)
Affects about 1 in 4 adults in Quebec. Often called the “silent killer,” hypertension typically has no noticeable symptoms, but it can gradually damage the arteries, heart, kidneys, and brain. Common causes include genetics, aging, obesity, physical inactivity, excessive salt intake, smoking, stress, and alcohol use
Management includes:
• Lifestyle changes: Reducing salt, losing weight, regular physical activity, managing stress
• Medications: Several types may be used to lower blood pressure safely
• Monitoring: Home blood pressure monitors and periodic clinic visits help track progress
Follow-ups are essential to prevent long-term complications such as stroke, heart failure, or kidney disease.
Palpitations
Palpitations are the sensation of a rapid, fluttering, or irregular heartbeat. They can feel like your heart is racing, pounding, or skipping beats. While often benign — especially when triggered by stress, caffeine, or fatigue — they can sometimes signal an underlying rhythm disorder.
Seek medical attention if palpitations are:
• Frequent, persistent, or worsening
• Associated with dizziness, chest pain, fainting, or shortness of breath
Evaluation may include:
• A physical exam and resting ECG
• A Holter monitor to record heart rhythms over 24–48 hours
• Blood tests or cardiac imaging
Atrial Fibrillation (AF)
AF is the most common heart rhythm disorder, especially in adults over 60. It causes the upper chambers of the heart to beat irregularly and ineffectively, increasing the risk of blood clots and stroke.
Symptoms may include:
• Palpitations
• Fatigue or weakness
• Shortness of breath
• Lightheadedness
However, many people have no symptoms and are only diagnosed during a routine ECG.
Diagnosis and management:
• ECG or Holter monitoring to confirm the diagnosis
• Blood thinners (anticoagulants) to prevent stroke
• Medications to control heart rate or rhythm
• In some cases, cardioversion or ablation may be recommended
Atherosclerosis
Atherosclerosis is the progressive build-up of plaque (cholesterol, calcium, and other substances) inside the arteries, narrowing them and limiting blood flow. It can affect the heart (coronary artery disease), brain (stroke), and limbs (peripheral artery disease).
Risk factors include:
• High cholesterol
• Smoking
• Diabetes
• High blood pressure
• Family history
• Sedentary lifestyle
Complications: angina, heart attack, stroke, or limb ischemia
Prevention and management:
• Healthy diet rich in fruits, vegetables, and whole grains
• Regular exercise
• Smoking cessation
• Cholesterol-lowering medications (statins)
• Blood pressure and diabetes control
Angina
Angina is chest pain or discomfort that occurs when the heart muscle doesn’t get enough oxygen-rich blood, usually due to blocked or narrowed coronary arteries.
Symptoms may feel like:
• Pressure, tightness, or burning in the chest
• Pain that radiates to the arms, jaw, neck, or back
• Triggered by physical exertion or stress, and relieved with rest
Types:
• Stable angina: Predictable, with exertion
• Unstable angina: More severe, occurs at rest — may be a warning sign of a heart attack
Treatment options:
• Nitroglycerin tablets for symptom relief
• Beta blockers or calcium channel blockers
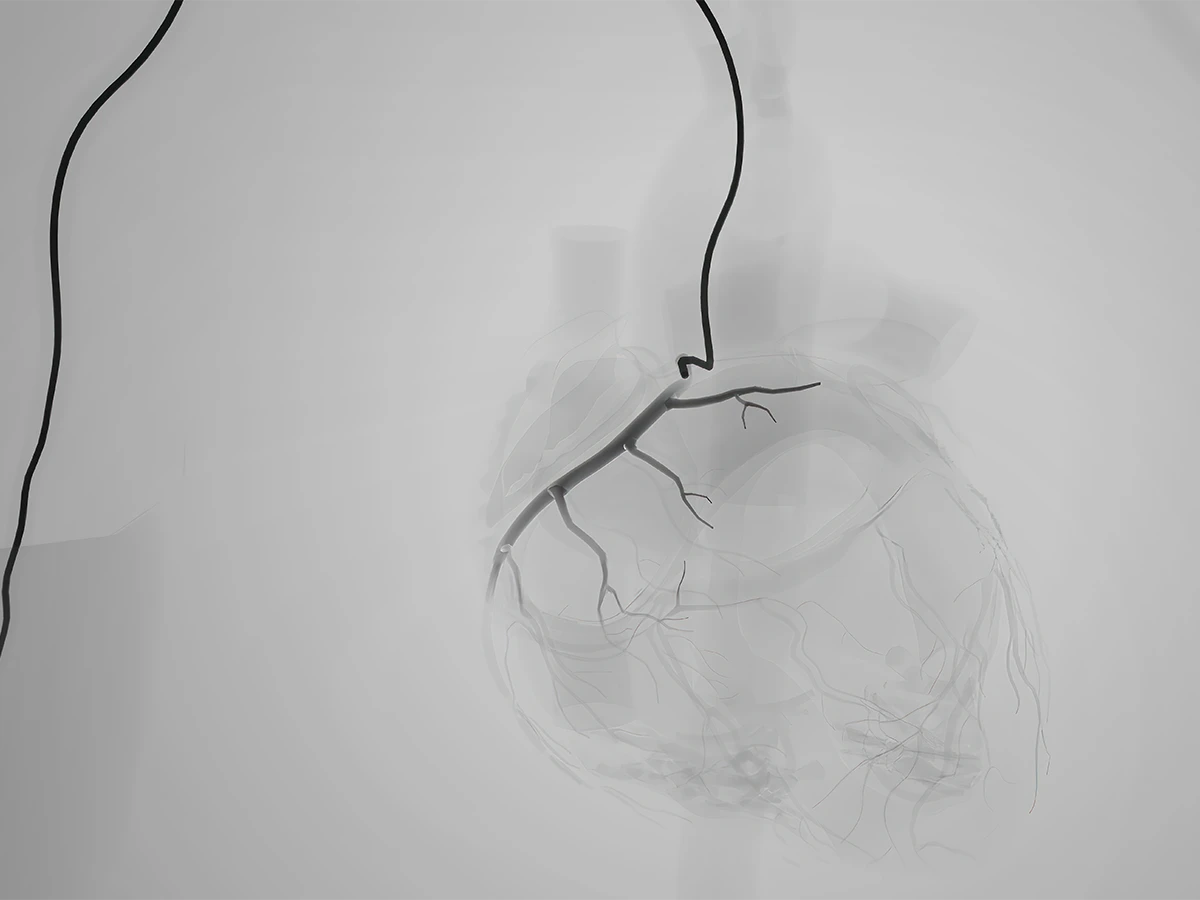
• Angiography and revascularization in severe cases
If chest pain is new, severe, or lasts more than a few minutes — call 911.
Myocardial Infarction (Heart Attack)
A heart attack happens when a coronary artery becomes completely blocked, depriving part of the heart of oxygen.
Symptoms may include:
• Crushing or heavy chest pain or pressure
• Pain that spreads to the left arm, neck, jaw, or upper back
• Shortness of breath
• Sweating, nausea, or dizziness
Women and older adults may have more subtle symptoms such as fatigue or indigestion.
What to do:
Call 911 immediately. Time is critical — early treatment can limit heart damage and save lives.
Treatment may include:
• Emergency angioplasty (stent)
• Medications (blood thinners, beta blockers)
• Long-term cardiac rehab
Heart Murmur
A murmur is an unusual sound heard during a heartbeat, caused by turbulent blood flow through the heart or valves. Many murmurs are innocent (harmless) and don’t require treatment.
However, a murmur may also signal:
• Valve disease (narrowing or leakage)
• Congenital heart defects
• Heart enlargement
Evaluation may include:
• Listening with a stethoscope
• Cardiac ultrasound (echocardiogram) to assess valve function and blood flow
Pericarditis
Pericarditis is inflammation of the pericardium, the sac surrounding the heart.
Symptoms:
• Sharp or stabbing chest pain that worsens when lying down or with deep breaths
• Relief when sitting up or leaning forward
• May be accompanied by fever, fatigue, or shortness of breath
Causes include viral infections, autoimmune diseases, heart surgery, or heart attacks.
Diagnosis: ECG, echocardiogram, and blood tests
Treatment: Anti-inflammatory medications (ibuprofen, colchicine), rest
Most cases resolve within days to weeks. Rarely, complications like fluid buildup or recurrence may occur.